Inguinal Hernia Repair: Laparoscopy Or Open?
Open access peer-reviewed chapter
Laparoscopic Inguinal Hernia Repair: Technical Details, Pitfalls and Current Results
Submitted: Dec 17th, 2022 Reviewed: Apr 3rd, 2022 Published: July 18th, 2022
DOI: 10.5772/intechopen.76942
IntechOpen Downloads
1,554
Total Chapter Downloads on intechopen.com
Abstract
Expanding view of minimal invasive surgery horizon reveals new practice areas for surgeons and patients. Laparoscopic inguinal hernia repair is an example in progress wondered past many patients and surgeons. Advantages in laparoscopic repair motivate surgeons to discover this popular field. In addition, patients search the nearly convenient surgical method for themselves today. Laparoscopic approaches to inguinal hernia surgery have become popular as a result of the development of feel near unlike laparoscopic interventions, and these techniques are increasingly used these days. As other laparoscopic surgical methods, experience is the nigh of import point in social club to obtain expert results. This chapter aims to show technical details, pitfalls and the literature results about two methods that are commonly used in laparoscopic inguinal hernia repair.
Keywords
- laparoscopy
- inguinal hernia
- TAPP
- TEP
*Address all correspondence to: fatihaltintoprak@yahoo.com
1. Introduction
For centuries, the inguinal hernias accept played an important office in the surgical literature and keep to preserve this feature today. With many procedures, inguinal hernia interventions go along to be the near common general surgery operations worldwide and approximately 2 million people are operated for inguinal hernia every year. There are many techniques described on the surgical treatment of inguinal hernias. There is no other example of disease preoccupied in the surgical literature. Existence of the postoperative complications suggests that we have not found the platonic handling option yet because a wide multifariousness of techniques have been described and virtually of the surgeons engaged in this procedure take completed learning curves a long fourth dimension agone. In 1984, almost hernia, Sir Astley Paston Cooper says: "No disease from the homo body, belonging to the surgeon, demands in its treatment, a improve mixture of precise, anatomical knowledge forth with surgical skill, compared to hernia in about of its variations". In this chapter, the details and results of two laparoscopic techniques, which have go mutual in inguinal hernia treatment today, are evaluated in detail.
Advertising
ii. Incidence and general data
The incidence of inguinal hernia varies according to age and sex. There is a bi-modal distribution in males and it increases in the first year of life and in older ages. The rate of 15% in the second decade increases with age and reaches 47% in the 7th decade. In females, this rate is iii% for life. In that location is a pregnant deviation between the male person/female ratio and is reported as one:15. Although the majority of the inguinal hernia patients exercise not face up neat problems in resuscitating their lives, the incidence of general incidence and emergency case incidence (incarceration-strangulation) increases with age [one].
Inguinal hernias are classified as direct or indirect inguinal hernia according to their machinery and anatomical characteristics. Indirect inguinal hernias are the most mutual subtype and the take a chance of strangulation is much higher compared to direct hernias. In the case of strangulation, it is besides necessary to mention that the femoral hernias head to this issue. Femoral hernias, which are found in seventy% of women and more often than not settled in the principle of "should be fixed when they are detected", due to the take a chance of strangulation, have not been included in this section [2].
When the side is concerned, it is a fact that all inguinal hernias are seen more on the right side. One of the theories developed to explain this is that there is anatomically protective outcome of the sigmoid colon present on the left side and delayed cloudburst of the processus vaginalis due to the slower descent of the scrotum on the correct side during embryological development.
Advertisement
3. History
The word "hernia" came from the Latin word "rupture" and was described every bit a disease in the first fifteenth century in papyrus. The idea of repairing surgery came out between fifteenth and seventeenth centuries although the inguinal region anatomy has been described in detail by Hesselbach, Cooper, Camper, Scarpa and Gimbernat during eighteenth and nineteenth centuries. In the twentieth century, "tension-gratis repairs" started to exist proposed and in the last 25 years, parallel to technological developments, videoscopic repairs became widespread. As a result of this development, surgical procedures have now get the standard procedure for "strengthening the abdominal wall in the transverse fascia plan" and are accepted all over the world [iii].
The thought of laparoscopic repair was outset declared by Ger in 1982 by the collapse of the internal loop. In 1990, Schultz used transperitoneal plugs and developed the intraperitoneal onlay mesh (IPOM) technique, which was performed in the same year past patching the Fitzgibbons peritoneum. Transabdominal preperitoneal (TAPP) patch application was first performed past Leroy in 1990. Then in 1991 Dulucq and in 1992 McKernan introduced full extraperitoneal (TEP) intervention [iv].
Advertisement
4. Anatomy
In the inguinal region, four different types of hernia—indirect, direct, femoral and obturator—can develop. One of the most important advantages of the posterior approach is the ability to reveal the entirety of hernia types. At that place are median, medial and lateral ligaments in the anterior wall of the belly after fetal period, followed by urachus obliteration, umbilical artery obliteration and inferior epigastric vessels, respectively. In addition, there are iliopubic tractus, pectineal ligament (Cooper) and lacunar ligament in pubic region, pubic tubercule, spina iliaca inductive superior (SIAS) and superior pubic ramus basic [5].
There are ii potential gaps in the preperitoneum. The "Bogros gap" is located between the transverse fascia and the peritoneum. Preperitoneal fatty tissue and porous connective tissue make full this area. The medial part of the preperitoneal cavity on the bladder is known equally the "Retzius cavity". The posterior view angle allows test of the myofektineal orifice, which is a relatively weak part of the abdominal wall and is divided by the inguinal ligament [half-dozen].
The external iliac vessels are anastomosed with the inferior epigastric vessels and the superior epigastric vessels. They supply the abdominal wall and penetrate the rectus abdominus through the cranial route within the vagina musculature rectus. Posteriorly inspected anulus inguinalis profundus will reveal the deep location of junior epigastric vessels. In addition, the abnormal obturator arteries formed past the anastomosis of the pubic ramus of the epigastric avenue with the obturator artery, known as "Corona Mortis", plant the basis of the death triangle. The medial side of this triangle is vas deferens, the lateral side is the spermatic cord and the posterior border is the peritoneal margin.
The inferolateral border of the iliopubic tract, the superomedial edge of the gonadal vessels and the lateral border of the peritoneal catheter is defined equally the surface area of the hurting triangle and the intermediate cutaneous branches of the lateral femoral cutaneous nerve, the femoral branch of the genitofemoral nerve and the anterior branch of the femoral nerve contain posterior anatomical arroyo.
Advertisement
5. Textile and methods
We performed laparoscopic inguinal hernia surgery in 163 patients between Jan 2022 and 2022 in our clinic. Laparoscopic hernia repair was recommended to patients who are suitable for general anesthesia, had no previous abdominal surgery or incarceration or strangulated hernia or without acute mechanical intestinal obstacle. In terms of learning curve, TAPP was performed on first 50 cases and TEP on the post-obit cases. A total of 155 (95%) patients were male and 8 (5%) were female. A full of 51 patients received TAPP (31.ii%) and 112 patients (68.seven%) received TEP. Eight patients who underwent TAPP (xv.6%) were operated for recurrence. Xiii patients (25.4%) underwent bilateral repair while 3 (five.eight%) patients underwent the same session umbilical hernia repair. The groups were evaluated in terms of operation time, pain scores, recurrence rates, duration of hospitalization and render to daily activity and complexity rates. TAPP average operation time is 58 min while in bilateral cases this duration is 72 min. The duration of operation of recurrent cases was 59 min average and there was no significant divergence between these patients and the principal cases. A total of 112 patients were treated with TEP technique. Nineteen patients (16.9%) were operated for recurrent hernia, and fourteen patients (12.5%) underwent bilateral repair. In three patients (2.6%), the aforementioned session umbilical hernia repair was also performed. Average elapsing of TEP is 47 min while in bilateral cases this duration is observed as elongated, 56 min. The elapsing of functioning in recurrent cases was 56 min and in that location was no significant difference between these patients and the primary cases. The hospital stay was measured equally 1.ii days for TAPP and 1.1 days for TEP, and no significant divergence was found between the groups. It was also found that the pain scores between the two groups were like as 3.2 and two.9 for TAPP and TEP, respectively. The time to return to the daily action for TAPP was five.6 days and for TEP was 5.3 days and no meaning deviation was plant betwixt the 2 groups. Every bit a complication, seroma in four patients (ii.4%), recurrent hernia in 2 patients (1.2%) and chronic persistent hurting in 6 patients (iii.6%) occurred. Patients with recurrence were reoperated. Five patients with chronic persistent hurting were treated with medical therapy within 6 months, and one patient with osteitis pubis was detected and curettage was performed past orthopedics clinic. In our study, no pregnant deviation in recurrence, return duration to work, pain score, duration of hospitalization and postoperative complication were detected between the groups.
Advertisement
6. Technical points
The use of laparoscopic methods for inguinal hernia surgery is advanced minimal invasive surgery with less tissue trauma, less postoperative pain, lower postoperative infection hazard and faster postoperative recovery. It is possible to combine positive furnishings such equally faster return to piece of work and better cosmetic results. Equally with all surgical techniques, minimally invasive techniques also have advantages. Compared to open surgery, some disadvantages of inguinal hernia surgery are the initial functioning time and the long learning curve. Also, the cost is relatively high. In addition, unlike open surgery, the lack of sense of depth in the paradigm, that is, the performance with the 2nd prototype requires the surgeon to boss the inguinal region anatomy at a loftier level. Instead of cost problem, by time, the integration of the learning curve and the increase in the feel reduce almost of the problems.
There are two primary techniques when laparoscopic inguinal hernia repair is concerned. These are defined as transabdominal preperitoneal approach (TAPP) and total extraperitoneal approach (TEP). Co-ordinate to the International Endohernia Grouping's 2022 Guidelines, revised in 2022, TAPP and TEP take become the preferred repair techniques for the Lichtenstein technique, peculiarly after hernia recurs by open pre-repair [7].
Advertizement
7. Laparoscopic transabdominal preperitoneal approach
It is stated that TAPP is the first method to be learned because it is applicable in all inguinal region hernia types. As an reward of the intraabdominal approach, the posterior wall anatomy tin be better dominated, then proper and adequate parietalization tin be made more comfortable. Compared to TEP, the cost is lower and the learning bend is shorter. TAPP is a highly successful method for both incarcerated and scrotal hernias. Due to intraabdominal vision, providing a wide field of view report is one of its greatest advantages and is a method that tin be used in laparoscopically repaired recurrent hernias.
Advertisement
viii. Technical details
8.1. Operating room layout
The opposite side of the surgical field and both legs are in airtight position. In bilateral hernia repair, both arms are in closed position. The videomonitor laparoscopy belfry is placed on the patient's foot, on the side to be operated. The operator can be placed on the contrary side of the area to be operated and the camera assistant can be placed on the same side or reverse side of the surgeon depending on the feel and habits of the team. We prefer the camera assistant to sit on the same side of the surgeon (Effigy 1).

Effigy 1.
Operating room: The surgeon and camera assistant placed on the opposite side of the surgical area.
8.two. Surgical instruments
-
Standard laparoscopic equipment consisting of photographic camera, monitor, light and bag
-
ten mm diameter and 30° angle camera
-
One 10 mm and two five mm in diameter totally iii trocars
-
Veress needle
-
Endoinstruments (Atraumatic pens, dissector, scissors, hook, acutenaculum, aspirator)
-
5 mm diameter vessel sealing device
-
fifteen × fifteen cm polypropylene or polyester special shaped patch
-
Fixing cloth for mesh detection and peritoneal closure (mechanical stapler, tissue adhesive or non-absorbable suture cloth) (Figure 2).

Figure 2.
Surgical instruments for TAPP process.
8.3. Preparation of the patient and treatment of trocars
A single dose of 1 g 2nd-generation cephalosporin equally condom antibiotic is injected one-half an hour before the onset of operation. The patient should urinate before performance and preoperative fluid resuscitation should exist kept to a minimum. Before the functioning, the patient is scrubbed and covered in the supine position for sterility. Under general anesthesia, by Hasson technique or with Veress needle which is placed in the infraumbilical region, produces caphno pneumoperitoneum. General intraabdominal exploration is completed with a ten mm trocar inserted in the infraumbilical region. The operating tabular array position is kept (30° Trendelenburg and 15°–20°opposite to the operating expanse). Two operating ports (5 mms) are placed on the umbilical level transverse line, with the lateral sides of both rectus muscles localized and placed under direct vision. The trocars on the operative side are placed on infraumbilical transverse line, while the opposite trocar is placed 4–5 cm caudal side on this line (Figure 3). In bilateral hernias, it is suggested that both trocars to be placed on the transverse line at the same level.
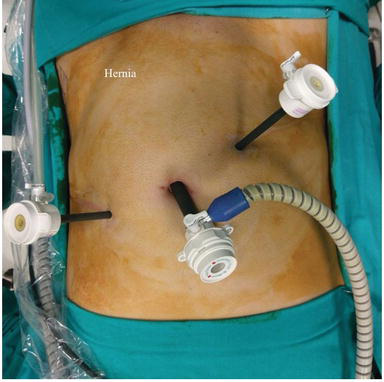
Figure 3.
Trocar placement for TAPP procedure.
8.four. Intraabdominal inguinal exploration
Every bit the trocar placements are complete, the inguinal area is examined with care. The hernia blazon is detected and the content—if present—of the hernia is carefully reduced to origin with atraumatic clamp. If at that place are elements such equally intestine or omentum in the hernia sac, the vitability of intestine or omentum is checked after reducement.
8.5. Peritoneal incision, dissection and grooming of preperitoneal area
The preparation of the peritoneal flap starts on approximately 5 cm to a higher place the hernia canal at the level of the inductive superior crista iliaca on the upper outer side of the annulus inguinalis. The incision is avant-garde to the medial side of the transverse airplane through the upper five cm of the inguinal canal's inner band and terminated at approximately 2 cm to median ligament.
The peritoneal incision tin be done with endoscissors or hooks. Remainder of the peritoneal flap on the inguinal culvert inner ring tin can exist hands disrupted with the assistance of intraabdominal CO2 pressure, stretched with endograsper. Peritoneal dissection, below the inguinal canal inner ring, is a little more difficult. The lower peritoneal flap is liberated until lateral visualization of the iliopubic tract, and medial visualization of the Cooper ligament. The hernia sac is advisedly dissected from the spermatic string and elements that are attached through the lower peritoneal membrane (Figure four). The peritoneal upper and lower flaps are dissected in each direction to provide large parietalization and vision of myopectineal orifice. Thus, plenty space is available to lay a mesh on likely direct, indirect and femoral herniation defect sources. If bilateral hernias are present, the peritoneal incision tin can exist extended from 1 side of the crista iliaca to the other side of the crista iliaca, but in the literature it is suggested that a single incision should be made and a peritoneal bridge could exist released in the midline.

Effigy 4.
Anatomic details of left inguinal region after peritoneal flap preparation.
eight.vi. Grooming, placement and detection of the mesh patch
Special shaped polypropylene or polyester patches prepared in size advisable to the anatomical characteristics of the hernia of the patient are used. The patch is rolled from the outside to the inside and from top to bottom in the class of a roll with limb or without limb (Figure five). It is placed into the abdomen through a 10 mm trocar. With the help of 2 endograspers, placed in the working ports, the roll is unfolded in the reverse direction and is laid to cover the existing hernia defect and potential hernia sources. Besides, it must be ensured that the patch is placed with a proper tension. When a limb patch is practical the lower limb is passed under the spermatic cord and it is wrapped in a tie and is joined laterally with the upper limb once again. The location and number of staples is very important for the immobilization of the mesh patch. The bones dominion—with dissimilar suggestions about this—is that the staples must be placed on the ileo-pubic tract. We prefer to set it with 2 absorbable staples totally, one medially to the Cooper ligament and one to the dorsum of the transverse fascia (Figure half dozen). Tissue adhesives or absorbable suture materials may as well be used for detection.

Figure five.
Mesh training.

Effigy 6.
Afterwards mesh fixation in TAPP procedure.
8.7. Closure of peritoneum over mesh
After the integration of fixation, the upper and lower leaves of the peritoneum are covered on the patch and the contrary edges are closed with either continuous stitches or with clips. Endmost the peritoneum with stitches is more than convenient simply requires more time and experience. The hernia sac, which is commonly left in the lower peritoneal sail and reduced into the peritoneum, can exist left if it is pocket-size, too the larger sacs can be partially resected before closing the peritoneal leaves. According to feel and preference, a drain can be placed behind the peritoneal flap. Afterward the peritoneum is closed, 5 mm ports are removed under direct vision and the operation is terminated.
8.8. Postoperative care
Oral intake can be started a few hours afterward surgery and the patient is mobilized the aforementioned evening. The post-obit day the patient can be discharged by removal of the bleed. In that location is no need to regulate postoperative medical treatment other than oral analgesics.
Advertizing
9. Laparoscopic full extraperitonal approach
Despite discussions about the apply of laparoscopy in the repair of primary unilateral groin hernias, the superiority of TEP in bilateral or recurrent hernias is accepted. The major advantages of this method are that it is extraperitoneal and there is no break in peritoneum. The dominance of the beefcake of the posterior wall is not as good as TAPP, simply sufficient parietalization is possible with TEP. Nowadays it becomes the beginning choice especially for athletes both men and women.
ix.1. Operating room layout
The opposite side of the surgical field and both legs are in closed position. In bilateral hernia repair, both arms are in closed position. The videomonitor laparoscopy tower is placed on the patient'due south foot, on the side to be operated. The operator tin exist placed on the opposite side of the area to exist operated and the photographic camera assistant tin can be placed on the same side or contrary side of the surgeon depending on the experience and habits of the team. We prefer the camera assistant to sit on the same side of the surgeon.
9.2. Surgical supplies
Standard laparoscopic equipment consisting of a camera, a monitor, a calorie-free and an insuflator
-
10 mm bore balloon trocar
-
Laparoscope with a bore of 10 mm and a 30° angle
-
A 10 mm, 2 5 mm diameter, totally 3 trocars
-
Atraumatic clamps, endodissectors, endoscissors, endohooks, endoclapms, endoaspirators
-
five mm diameter vessel sealing device
-
xv × xv cm polypropylene or polyester special shaped patch
-
Fixation fabric (mechanical staple or tissue adhesive)
ix.three. Training of the patient, application of extraperitoneal trocars
A unmarried dose of 1 g 2d-generation cephalosporin as safety antibiotic is injected half an hour before the onset of operation. The patient should urinate earlier operation and pre-operatory fluid resuscitation should be kept to a minimum. With full general anesthesia, the operation starts in supine position. In method of TEP, the patient should be wider painted than the TAPP technique, from the nipple to the perineum. Infraumbilical, slightly lateralized incision is made on the hernia side and so the rectus sheath is opened by transverse incision. Rectus fibers are removed with Farabeuf retractor and edgeless dissection is performed to reach the Bogros area. A tunnel is made between bellybutton to pubis. In front of this tunnel, there is a parietal peritoneum from the dorsum of the rectus muscle and from the finish of this fascia to the transverse form of the linea semilunaris. After edgeless dissection and cannula is completely inserted from the preperitoneal tunnel to the pubis, it is removed from the trocar cannula and replaced with a telescope, and the cannula is inflated with a balloon attached to the mandrel. Air is discharged xx–25 times with puar subsequently waiting for thirty s and this process is repeated iii times. With some balloons, it is possible to view within with scope as it inflates. It can also be monitored whether the definite surgical area is viewed during this observation. Upper view of rectus fibrils and lower view of parietal peritoneum indicates the right position. A x mm trocar is placed in the infraumbilical incision to preclude gas leakage and the telescope is placed. The preperitoneal infinite is inflated with ten–12 mmHg COii. Two 5 mm ports are placed at a distance of 5 cm from the midline in direct view (Figure 7).

Figure 7.
Trocar placement for TEP process.
9.4. The dissection of extraperitoneal area and herniated sac
Subsequently the 30° camera is inserted, the inferior epigastric artery and vein are observed along the bottom of the rectus muscle. The parietal peritoneum is dissected in the medial and lateral directions to remain underneath. The Cooper ligament is visible in the inferomedial area and information technology is removed. The lateral attribute of the rectus is up to the edge of the crista iliaca and the fascia transversalis is opened with blunt and sharp dissections posteriorly. The potential hernia areas are examined and the hernia blazon is determined (Effigy 8). In the indirect inguinal hernia, the hernia sac is constitute adhered to the spermatic cord. The hernia sac should be dissected from the pubic tuberculum to the level of the external iliac vein. Large scrotal or indirect hernia may exist released past Zig technique if it is confirmed that the hernia sac does not incorporate omentum or intestinal contents. The anatomic regions described equally Femoral and Hasselbach triangles should be examined in terms of direct and femoral hernia that may be accompanied. The ililopubic tract must be detected not to injure the femoral and lateral femoral cutaneous nerves of the underlying genitofemoral nerve. The lateral dissection does not need to be equally wide as the TAPP technique. The hernia sac should exist gently released and reduced from the spermatic string and cremaster fibers. If the peritoneum is wounded during the dissection procedure, the defect can exist airtight with a prune. If gas insufflation flows through the gap to the peritoneal defect, the enlarged abdomen will restrict the area of dissection. In order to foreclose this, intraperitoneal air could be taken out from the upper left quadrant of the midclavicular line through the abdominal cavity (Palmer'due south betoken) with Veress needle. The valve is left open, the evacuation of the gas is provided and the operation can exist continued.

Figure eight.
Potential hernia areas for TEP process.
9.5. Grooming, placement and detection of the mesh patch
Special shaped fifteen × 15 cm polypropylene or polyester patch can exist used according to the anatomy of the patient. The patch can exist prepared with limb or without limb. Information technology is rolled upwardly from the top and laid to the extraperitoneal space by the x mm camera trocars. With the assist of two endograspers placed in the working ports, the patch is unfolded in the contrary direction and is laid to embrace the existing hernia defect and potential hernia areas. It should exist ensured that the area where the patch is applied covers it with a proper tension. When a limb patch is applied, the lower limb is passed nether the spermatic cord and it is wrapped in a tie and is laterally joined to the lower limb (Figure 9). The lower border of the patch is placed so that it remains at least two cm in a higher place the released hernia sheath. The locations and numbers are very important if the absorbable staple is preferred for the detection of the mesh. The basic rule, with dissimilar suggestions almost this, is that the mesh must be placed on the ileo-pubic tract. We prefer to fix it with a full of ii absorptive staples, ane medially to the Cooper ligament and 1 to the dorsum of the transverse fascia laterally. On the lateral edge of the spermatic cord there are anatomical areas defined as the triangle of pain mentioned to a higher place and the death triangle at the medial edge. Staples must be avoided in these areas. Tissue adhesives have also been used today as fixing cloth. The use of drains varies according to experience and habits. We routinely utilise aspirative drain later on TEP.
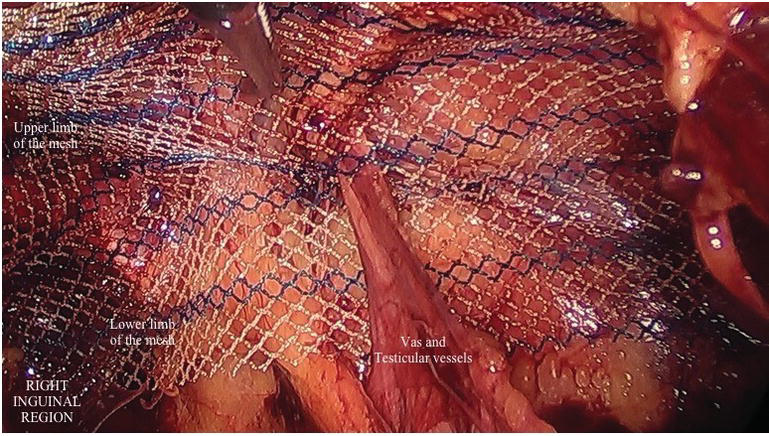
Effigy 9.
Later mesh fixation.
9.6. Postoperative care
Oral intake tin exist started a few hours afterward surgery and the patient is mobilized the same evening. The following mean solar day the patient can be discharged by removal of the drain. There is no need to regulate postoperative medical treatment other than oral analgesics.
Advertisement
ten. Pitfalls
In this chapter, details have identify as noted; details in electric current practice are given while applying the laparoscopic hernia repair. The points to exist considered are evaluated for both techniques. In addition, the difficulties faced by the surgeon are itemized.
ten.1. TAPP
-
As all laparoscopic operations, the offset point to notation in laparoscopic hernia surgery is trocar entry sites. Correct positioning of the appropriate points will foreclose intestinal injuries that may occur at the fourth dimension of start entry and bleeding which may exist caused past the injury of the abdominal wall, particularly the epigastric vessels.
-
A complete exploration should be washed in terms of hernia type, size, presence of accompanying incarceration and other pathologies in intraabdominal exploration.
-
Taking enough width for dissection during the preparation of the peritoneal flap volition ensure that the exploration expanse is convenient. Working on a sufficient width of dissection will facilitate the spread of the patch, the adequate closure of the hernia defect and the operator's work during the detection of the patch.
-
A very careful dissection should be performed in order to avoid damage to the spermatic cord structures, peculiarly in the presence of indirect hernia, when the hernia incision is dissected, as interference with the anatomical planes may result in attempts made for recurrent hernia.
-
Should be very careful non to hold Vas Deferens past endo-devices so equally to not disturb.
-
The autopsy should be performed at an adequate width of the myopectinale opening, but should be avoided from the extreme dissection in front end of the psoas site in the lateral direction. There is an anatomic area defined as triangular pain in this region and it should be especially noted that the cutaneous femoral lateralis and femoral branches of genitofemoral nerves are not damaged. Postoperative chronic pain syndromes tin be encountered in the event of a possible nerve injury.
-
Death triangle is divers as the anastomotic area between the external iliac vein and the obturator vein and should exist avoided from the farthermost autopsy. Considering, in the event of a possible vascular injury in this region, catastrophic consequences may be encountered.
-
The staples used for patch detection due to the same reasons should never be used nether the iliopubic tract.
-
Should be sure to identify the staples on the medial side, especially on the Cooper ligament, so that postoperative osteitis pubis is avoided.
-
It is by and large brash to use the least amount of other materials that tin exist used for stapling or patch fixation.
-
Wide laying of the mesh will reduce the recurrence rate by covering the 3 hernia areas.
-
Reducing the intraabdominal CO2 pressure during the peritoneal flap closure and correcting the patient's position volition facilitate closure because it volition reduce tension. The effective endmost of the flap is important to forestall postoperative intestinal adhesions.
10.2. TEP
-
The infraumbilical incision should be made from slightly left or right lateral. What should be noted here is to be on the rectus front sheath. If the linea alba is opened by mistake, the gas will menstruation to the intraabdominal region and strengthen the technique at the start.
-
It is important to discover the bright white color of the rectus posterior sheath, and it is important that the balloon is inflated by advancing the balloon trocar in this space. The balloon dissection between the fibers of the rectus will crusade haemorrhage between the muscle fibers, disturbing the dissection plans and preventing the vision.
-
If gas flows into the abdomen during possible peritoneal injuries in the TEP technique, as mentioned in the techniques section, the gas must be evacuated with the Veress needle, which volition be entered from the Palmer point.
-
Big peritoneal defects may cause postoperative patchy contact with the intestines and lead to postoperative abdominal adhesion development. For this reason, large peritoneal defects should exist closed with endoclips.
11. Complications and direction
In this section, complications related to laparoscopic inguinal hernia surgery, literature information virtually management of these complications and suggestions based on our own experience are included.
11.ane. Local complications
The almost common complications are serous fluid deposits (seroma) and haemorrhage(hematoma) which may develop during operation. Patients should exist informed in the preoperative menstruum near these complications. Postoperative seromas normally resorb spontaneously inside ii weeks and do not require handling. Therapeutic drainage needs arise in the presence of seroma persistent for longer than vi–8 weeks or in the presence of seroma causing clinical symptoms. The use of peroperative aspirative drains in risky patients of who may be predicted seroma and hematoma development may prevent the development of these complications. Scrotal height is recommended in the postoperative flow. If intestinal wall ecchymosis occur, mechanical pinch, cold application and medical treatment tin can be tried. Subcutaneous emphysema is often untreated and spontaneous. In rare occasional hydrocele cases, it will be more appropriate to consult with a urologist.
11.two. Neurological complications
The treatment of chronic pain syndromes subsequently laparoscopic hernia surgery is often long and difficult. Chronic postoperative pain has been reported in up to 63% of all groin repairs and significantly affects clinical outcomes. The pain following laparoscopic surgery is ordinarily neuropathic pain. The cause is usually the damage or trapping of the lateral femoral cutaneous or femoral branch of the genitofemoral nerve. Clinically it occurs equally acute called-for and/or crushing hurting in a particular dermatome. Mareljia parestetika is the name of a pain clinic that develops after a lateral femoral cutaneous nerve injury and persistent paresthesia lateral of the femoral surface area. It is recommended to use corticosteroids or anesthetic injections which tin can be applied at residuum, cold application, NSAIDs, concrete therapy, locally. Osteitis pubis is; the name of the pain clinic that occurs due to public inflammation and arises particularly on the heart of the groin or on the pubis, especially with femoral adduction. Diagnosis can be made by excluding recurrent hernia diagnosis radiographically and performing os imaging. The treatment approach is the same as neuropathic hurting. Often, six months are required to respond to treatment. Yet, if the cure is not bachelor, the orthopedic consultation may be needed to consider possible bone resection or curettage options.
11.3. String and testicular injury
Ischemic orchitis should exist considered in the complaints of hardened, enlarged and painful testicles that announced nigh 10 days afterwards the repair of the inguinal hernia. Information technology is often self-limiting. It is usually the result of a possible damage to the pampiniform plexus, non the testicular artery. Ultrasound can distinguish necrosis or ischemia. If testicular necrosis is detected, urgent orchiectomy may be necessary. Treatment includes 4 hydration and NSAIDs. If testicular artery is damaged, information technology tin exist caused testicular cloudburst after long periods of operation. Vas deferens may not exist manipulated during surgery and maximum effort to avoid agonizing their diet may help to avert these complications.
xi.iv. Recurrents
Postoperative pain, swelling and the presence of a mass in the inguinal region should exist considered. Diagnosis can be made past radiological examinations. Technical factors that play a office in the development of recurrence include inappropriate patch size, inadequate patch, stress or inaccurate detection, lack of experience, tissue ischemia and infections. Factors related to the patient include malnutrition, obesity, wound healing disorders and uncontrolled diabetes mellitus. Surgical intervention should exist considered in the treatment.
Other complications include urinary retention, which tin can be prevented by the patient's urination earlier surgery or by peroperative urinary catheterization. Paralytic ileus, visceral injuries, vascular injuries, intestinal obstacle, hypercapnia, pneumothorax and gas embolism are likewise uncommon complications.
12. Literature review
The results of laparoscopic and open inguinal hernia surgeries are now existence compared very much. Postoperative hurting complications, recurrence rates, patient satisfaction, cost analysis are oft discussed. Papachariston and colleagues in their postoperative evaluation of pain study [8], even though information technology was reported to require more analgesic in the first 6 h in the TAPP group, pain was reported in 2–11% of the open surgery group and reported equally one–4.2% in the laparoscopic group. In the same study, persistent hurting lasting from seventh day to one year in the open surgical grouping was associated with postoperative fibrosis, while point pain in the laparoscopic group was associated with scar tissue rupture. In a meta-assay evaluating persistent pain [ix], patch repair has been shown to reduce persistent pain as opposed to pain relief, and it has likewise been constitute that chronic pain is less in the laparoscopic method.
In a study in which approximately x,000 patient outcomes were assessed in the U.s. and patients were followed for 3 years [10], the recurrence rate of the laparoscopic method was found to be 0.iv%, and information technology was emphasized that the near of import difference between open up and laparoscopic operations was the achievement of sufficient experimentation, the number of operations performed. Co-ordinate to this recommendation, a randomized controlled trial conducted by the Veterans Affairs Cooperative Written report and reporting of 2-year follow-ups [eleven], recurrence rates were reported as x% for laparoscopic repair and five% for open repair, but after 250 laparoscopic cases techniques, results were improved. In a more contempo study, Lal et al. [12] has shown that surgeons accept reduced recurrence rates from 9 to 2.nine% later on 100 operations. In different studies, it has been reported that the laparoscopic techniques are spreading and the time to appraise the competence of the surgeons is betwixt 50 and 100 cases. A meta-analysis by Köckerling et al. [xiii] evaluating the human relationship betwixt patch fixation and recurrence, cases that patch fixation was performed and in cases not performed, at that place was no departure in the elapsing of operation, patch-related complications, recurrence and duration of hospital stay.
In a randomized controlled meta-assay in which Wei and colleagues evaluated the outcomes of 1000 patients published in 2022, there was no difference betwixt the 2 surgeries, hurting score, operation fourth dimension, return to daily activity, hospitalization time, complication and cost between the two surgeries. In conclusion, TEP was found to exist more complicated than TAPP and advised to start laparoscopic surgery with TAPP to inexperienced surgeons [14]. In a study published past Köckerling et al. [15] there was no difference between 2 surgeries in terms of intraoperative complications and reoperation rates. However, after TAPP surgery, complication rates were found to be higher due to possible big complications, more scrotal hernia, elderly patient pick.
In a study conducted by Payne et al. [16] to mensurate postoperative quality of life, it has been shown that patients' compliance with straight leg exercises is improve afterwards laparoscopic surgery. Designed in the same way and studied by Lawrence et al. [17], this difference was more than evident in bilateral hernia repair.
The problem of cost is still an important trouble, with the fact that it has been removed from the large picture compared to the by. In the study conducted by Stylopoulos et al. [18] in 2003 and the results of 1.5 million patients evaluated, laparoscopic operations take been claimed to reduce costs compared to long-term open up surgery when salary, health insurance costs, reduced job quality, delayed piece of work shifts and the salary of the worker looking after the patient are taken into consideration. Farinas et al. [xix] showed that 60% reduction in indirect costs could be achieved despite the xl% increase in the direct costs of using non-dispensable devices and shortening of the performance time.
When TEP and TAPP were compared, there was no difference between the 2 techniques in terms of hospitalization time, recovery time and short term recurrence rates. The elapsing of the TEP technique is shorter than that of the TAPP technique [20]. Still, according to the International Endohernia Clan, information technology has been suggested that surgeons should apply the TEP technique later learning the TAPP technique and acquiring a sure experience in the learning curve [21].
In our written report, we have institute that there is but a minimal difference between TAPP and TEP techniques, in terms of operative fourth dimension. There was no departure in both techniques when recurrence, render to work, pain score, duration of hospitalization and complications were evaluated. Especially, we observed that bilateral and recurrent hernia had high patient satisfaction. Also nosotros observed that TAPP surgery in the early stages of surgery, shortened the learning bend.
In determination, laparoscopic inguinal hernia surgery takes place in daily exercise every bit an increasingly widespread upwardly-to-date treatment method in which preparation and experience gained over fourth dimension and patient satisfaction of clinical outcomes are very good.
Conflict of involvement
The authors declare that they accept no conflict of interest.
References
- 1.
Wagner JP, Brunicardi CF, Amongst PK. İnguinal Hernias Schwartz'south Princeples of Surgery. tenth ed. In: Brunicardi CF, editor. New York: In chief. McGraw Loma publishing; 2022. pp. 1510-1517 - 2.
Mark A, Malangomi and Michael J. Dosen Hernias Sabiston Textbook of Surgery: The biological footing of modernistic surgical practise 19th ed. In: Townsend CM, Beauchamp RD, Evers BM, Matteox KL, editors. London: Saunders publishing; 2022. pp. 1114-1141 - 3.
Van Hee R. History of inguinal hernia repair. Turnalul de Chirurgie. 2022; 73 :301-314 - 4.
Sachs M, Damm 1000, Enche A. Historical evaluation of inguinal hernia repair. World Journal of Surgery. 1997; 21 (2):218-223 - 5.
Bianutto SN, Repetto E, Aliendo MM, Borginho VW. İnguinal canal development: The muscular wall and the office of the gubernaculum. Clinical Beefcake. 2009; 22 (5):614-618. DOI: 10.1002/ca.20820 - six.
Rosenberger RT, Loewneck H, Meyer Thou. The cutaneous nerves encountered during laparoscopic repair of inguinal hernia: New anatomical findings for the surgeon. Surgical Endoscopy. 2000; 14 (eight):731-735 - seven.
Brittner R, Montgomery MA, Arregui, et al. Erratum to: Update of guidelines on laparoscopic(TAPP) and endoscopic (TEP) treatment of inguinal hernia (İnternational Endehernia society). Surgical Endoscopy. 2022; 29 (six):1655-1656. DOI: ten.1007/s00464-015-4156-three - eight.
Papachariston EA, Mitselou MF, Finokaliotis ND. Surgical outcome and infirmary cost assay of laparoscopic and open tension free hernia repair hernia. 2002; six (2):68-72.PMID:12152642 - 9.
European union Hernia trialists Colloboration. Repair of groin hernia with constructed mesh: Meta analysis of randomized controlled trials. Annals of Surgery. 2002; 235 (3):322-332.PMID:11882753 - 10.
Felix EL, Harbestson N, Vartanian S. Laparoscopic hernioplasty; significant complications. Surgical Endoscopy. 1998 April; thirteen (4):328-331. PMID:10094740 - 11.
Neumayer Fifty, Giobbie-Hurder A, Jonasson A, et al. Veterans cooperative studies program 456 investigators. Open mesh versus laparoscopic mesh repair of inguinal hernia. The New England Periodical of Medicine. 2004; 350 (xviii):1819-1827. DOI: 10.1056/NEJMoa 040093 - 12.
Lal P, Kajla RK, Chander J, et al. Laparoscopic total extraperitoneal (TEP) inguinal hernia repair: Overcoming the learning curve. Surgical Endoscopy. 2004; xviii (four):642-645. Epub 2004. DOI: 10.1007/s00464-002-8649-5 - 13.
Köckerling F, Jacob DA, Chowbey P, et al. A meta-anlysis examining the use of tucker fixation versus no-fixation of mesh in laparoscopic inguinal hernia repair. International Journal of Surgery. 2022; 10 (6):325. DOI: 10.1016/J.ijsu. 2022.04.014 - xiv.
Fx W, Zhang YC, Han Westward, et al. Transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) for laparoscopic hernia repair: A meta-analysis. Surgical Laparoscopy, Endoscopy and Percutaneous Techniques. 2022; 25 (5):375-383. DOI: 10.1097/SLE.0000000000000123 - fifteen.
Köckerling F, Bittner R, Jacob DA. TEP versus TAPP: Comparision of the perioperative outcome in 17.587 patients with a master inguinal hernia. Surgical Endoscopy. 2022; 39 (12):3750-3760. DOI: 10.1007/s00464-015-4150-9 - 16.
Payne JH, Grininger LM, Izawa WT, et al. Laparoscopic or open inguinal hernioraphy? A randomized prospective trial. Archives of Surgery. 1994; 129 (9):973-979. PMID:8080380 - 17.
Lawrence K, Mc Whinnie D, Goodwin A, et al. Randomized controlled trial of laparoscopic versus open repair of inguinal hernia: Early results, BMJ. 1995; 311 (701):981-985.PMID:7583639 - 18.
Stylopoulos Northward, Gazelle GS, Rattner DW, et al. A cost-utility analysis of handling options for inguinal hernia in 1,513,008 adult patients, Surgical Endoscopy. 2003; 17 :180-189. DOI: 10.1007/900464-002-8849-z - 19.
Farinas LP, Griffin FD. Toll containment and totally extraperitoneal laparoscopic herniorraphy. Surgical Endoscopy. 2000; 14 (1):37-40. PMID:10653233 - 20.
Qıu K, Ma J. Comments on TAPP versus TEP for laparoscopic hernia repair: A meta-analysis. Surgical Laparoscopy Endoscopy and Percutaneous Techniques. 2022; 26 (2):171. DOI: 10.1097/SLE.0000000000000251 - 21.
Bittner R, Köckerling F. Endorsement of the hernia surgical guidelines by the International Endohernia Society. Hernia. 2022; 22 (one):179. DOI: 10.1007/s10029-017-1674-z
Submitted: December 17th, 2022 Reviewed: April 3rd, 2022 Published: July 18th, 2022
© 2022 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Eatables Attribution 3.0 License, which permits unrestricted employ, distribution, and reproduction in whatsoever medium, provided the original work is properly cited.
Source: https://www.intechopen.com/chapters/61331
Posted by: haltermanorpostance.blogspot.com


0 Response to "Inguinal Hernia Repair: Laparoscopy Or Open?"
Post a Comment